4 Powerful Ways Midlife Stress Triggers Alzheimer Risk: What Science Reveals
Introduction
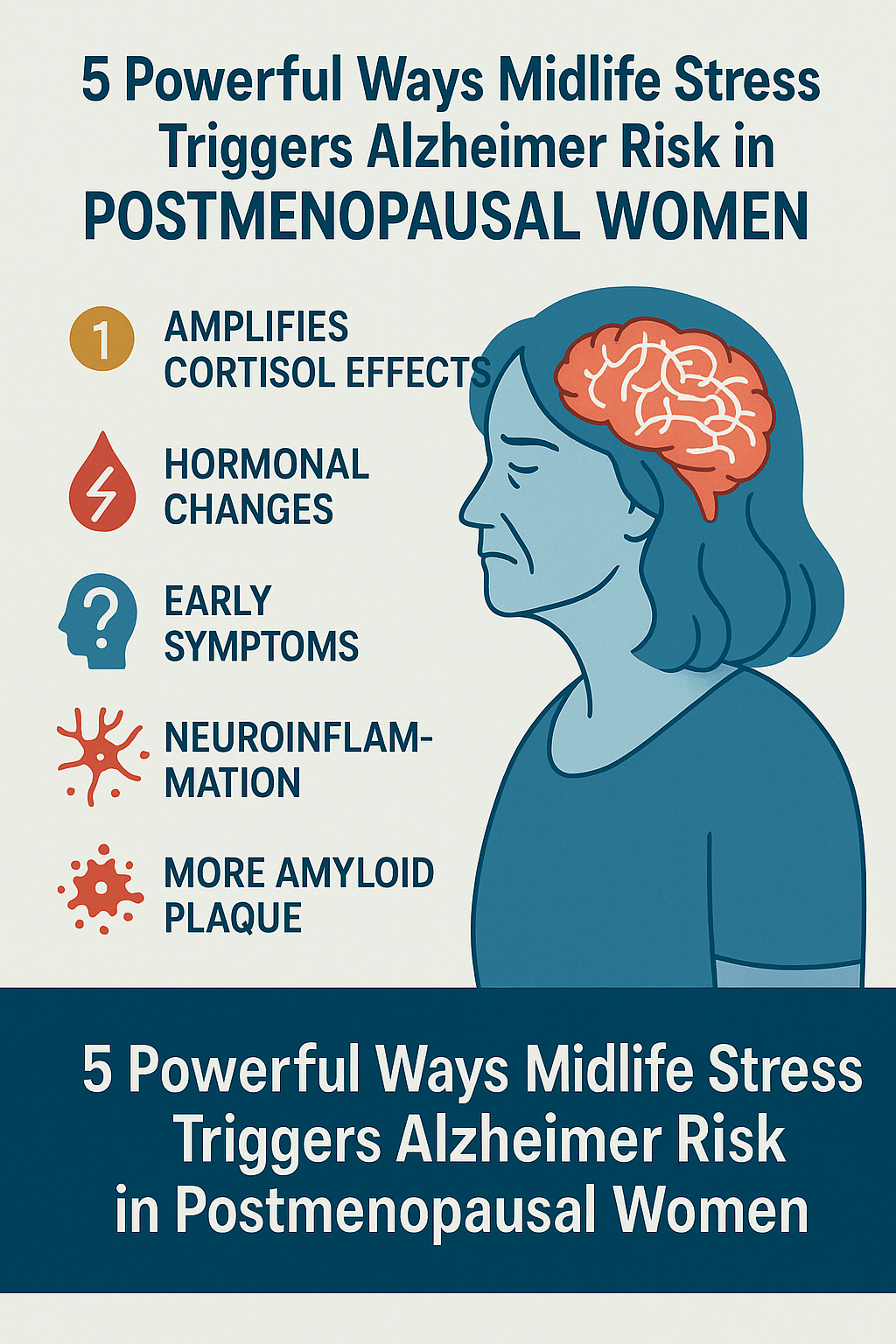
Stress is often described as the “silent killer,” but its impact may go deeper than previously understood—especially for women in midlife. A groundbreaking study published in the journal Alzheimer’s & Dementia has revealed a strong link between high levels of midlife stress and an increased risk of Alzheimer’s disease in postmenopausal women. This revelation sheds light on how hormonal changes combined with chronic stress can elevate the brain’s vulnerability, potentially setting the stage for long-term cognitive decline.
This blog will dive deep into the latest findings, break down the biological mechanisms behind the phenomenon, and offer actionable tips to reduce stress and support brain health during and after menopause.
1. Understanding the Link: How Midlife Stress Impacts Alzheimer’s Risk
According to a recent study analyzing data from 305 cognitively unimpaired women in Massachusetts, USA, postmenopausal women who reported higher levels of midlife stress showed increased risk factors for Alzheimer’s. The researchers found that stress hormones—particularly cortisol—had amplified effects due to hormonal changes after menopause. This amplifies their impact on amyloid, a protein closely associated with Alzheimer’s pathology.
Key Insight:
Postmenopausal changes may magnify the brain’s response to stress, increasing inflammation and promoting amyloid plaque build-up—both of which contribute to Alzheimer’s disease.
2. The Role of Cortisol: Why Stress Hormones Matter More After Menopause
Cortisol, the body’s primary stress hormone, is known for its role in the fight-or-flight response. However, elevated cortisol over long periods can impair memory, shrink parts of the brain like the hippocampus, and disrupt sleep—all known contributors to cognitive decline.
Why Postmenopausal Women Are More Vulnerable:
- Estrogen Decline: Estrogen helps regulate the stress response. After menopause, when estrogen drops, cortisol levels can spike more easily and remain elevated longer.
- Neuroinflammation: Chronic stress fuels inflammation in the brain, which exacerbates neurodegenerative processes.
Study Findings:
Women with higher cortisol levels showed higher amyloid activity, suggesting a direct link between stress biology and Alzheimer’s development.
3. The Hidden Culprit: How Hormonal Shifts Amplify Cognitive Risk
Menopause triggers a cascade of hormonal changes that affect brain chemistry. Estrogen, known to be neuroprotective, declines significantly. This not only impacts mood and memory but also weakens the brain’s defense mechanisms against stress and age-related decline.
How This Impacts the Brain:
- Reduces synaptic plasticity (the brain’s ability to adapt and learn)
- Increases vulnerability to toxins and free radicals
- Weakens the blood-brain barrier, allowing more cortisol to penetrate the brain
Combined with high midlife stress, these hormonal changes can act like a “double whammy,” pushing the brain into a prolonged state of cognitive vulnerability.
4. Warning Signs: Early Symptoms to Watch Out For
Many women attribute memory lapses or mental fog in midlife to “normal aging” or hormonal imbalance. However, these may also be early red flags of cognitive decline. Recognizing symptoms early can be key to prevention.
Common Early Symptoms:
- Forgetting familiar names or routines
- Difficulty concentrating or multitasking
- Mood swings, irritability, or anxiety
- Trouble with organization and time management
If these symptoms persist or worsen, they should not be ignored, especially if combined with chronic stress or sleep issues.
Expert Opinions
Dr. Lisa Mosconi, a neuroscientist specializing in women’s brain health, emphasized:
“The female brain ages differently. We cannot ignore how menopause changes its structure, chemistry, and vulnerability—especially under stress.”
Conclusion
The study connecting midlife stress to Alzheimer’s in postmenopausal women serves as a powerful reminder: stress is not just an emotional burden—it’s a biological threat. With menopause already tipping the hormonal scale, unmanaged stress adds fuel to the fire.
However, knowledge is power. By recognizing early symptoms, reducing stress, and adopting protective strategies, women can take control of their brain health and age with clarity, confidence, and strengt

